$20 Bonus + 25% OFF CLAIM OFFER
Place Your Order With Us Today And Go Stress-Free
This case raises the main problems of failing to recognise and respond to Roy Jacobs' deteriorating state where the Q-ADDS (Queensland Adult Deterioration Detection System) tool, as a nursing tool, is inadequately employed. The Q-ADDS tool was used to document observations but was not used with appropriate rigor to escalate the care needed.
Q-ADDS was also not seen as a clinical decision-making tool by the medical officers but was used more or less as a nursing tool. The result was that the medical and nursing teams had different understandings about what was required to occur with clinical escalation ultimately causing the death of the patient.
Also, the issue of compliance to the early warning systems was broader when the Darling Downs Hospital and Health Service’s compliance to such systems was reviewed, as it was the third similar incident in the region.
This standard highlights the importance for clinical governance frameworks that safeguard the provision of high quality and safe care (Australian Commission on Safety and Quality in Health Care, 2024). This case draws attention to the lack of clinical governance in particular, in relation to the process of managing clinical deterioration.
So, although the Q-ADDS tool was understood and applied by all but medical officers, these responsible nurses did not have a system of work in place where the Q-ADDS tool was used properly by all clinical staff. While the Q-ADDS scoring did serve a valuable purpose in ranking patients at risk for an adverse event, the failure to link clinical decisions to the Q-ADDS scoring missed opportunities for early intervention, and perhaps saved the patients’ lives.
These standard demands that communication is effective at critical points in care (Australian Commission on Safety and Quality in Health Care, 2024b). In this case communication of Roy Jacobs’ deteriorating condition between nurses and medical officers was not proper. Recording Q-ADDS scores should have been a positive, but being effective with it should also have involved results affecting clinical decisions. Patients’ poor outcome was attributed to the lack of communication around clinical escalation procedures.
This standard is concerned with quick recognition and response to acute deterioration (Australian Commission on Safety and Quality in Health Care, 2024c). This standard was violated directly by failing to escalate care on Roy Jacobs based on his deteriorating condition. The Q-ADDS tool and its associated clinical actions should have been properly applied so intervention would have occurred immediately and perhaps averted his death.
As per Australian Commission on Safety and Quality in Health Care (2024c), a systemic problem must be addressed through better training and practice of standard protocols, by ensuring that the medical and nursing staff act on clinical deterioration when signs of deterioration are not acted on.
A critical change is the requirement to enhance the hospital’s clinical escalation protocols based on the Recognising and Responding to Acute Deterioration Standard (NSQHS Standard 8) (Australian Commission on Safety and Quality in Health Care, 2024c).
In addition to recording patient observations, the Q-ADDS tool must not only be used to trigger mandatory actions, but such also as contacting senior medical officers when thresholds are breached.
This needs clear documentation and how to escalate based on deteriorating scores. As per Augutis et al. (2023), early warning tools must be used in combination with comprehensive training of clinical staff on the use of these tools and what to do post such patients as Roy Jacobs – those with acute conditions such as pneumonia.
Another essential change relates to improving communication among staff from different professional teams, in particular nurses and medical officers, work under the Clinical Governance Standard (NSQHS Standard 1) and Communicating for Safety Standard (NSQHS Standard 6) (Australian Commission on Safety and Quality in Health Care, 2024b).
Such structured interprofessional training programs in the use of early warning systems (such as Q-ADDS) and a culture of shared responsibility can be achieved. Nursing and medical staff need to understand their responsibility in handling clinical deterioration and clinical handover protocols must have built in tools to escalate and act on critical information at speed (Park and Kellerman, 2024).
Also, there must be ongoing monitoring of compliance with early warning and escalation process, and immediate feedback to staff when compliance is not met to support continuous improvement.
Also Read - Nursing Care Plan Assignment Help
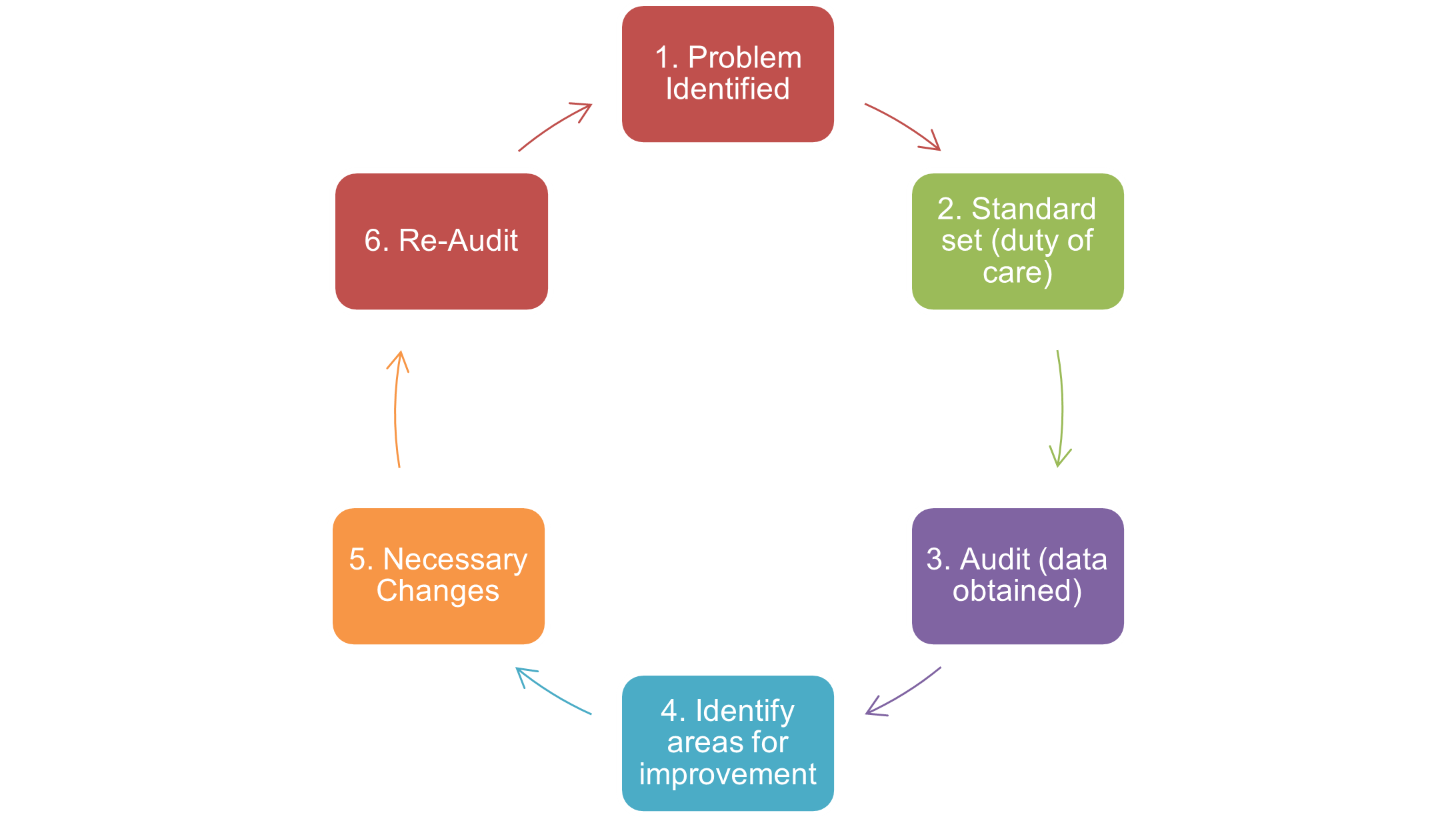
Analysis of the cause's contributing factors of a medical error are an important component of preventing further similar events. Complete the quality improvement table (below) in relation to the coroner’s case recommendations.
Students are required to identify 3 nursing interventions as part of the project plan
| Aim of the quality improvement: To promote opportunities for recognition, response to acute patient deterioration, adherence to early warning systems, and interprofessional communication to anticipate recurrent clinical failures | ||
| Nursing intervention to make change: | Expected outcome of the intervention: | Evaluation: How can this outcome be analysed in the future: |
| Intervention 1: Comprehensive Q-ADDS Training: Nursing and medical staff should be trained in the details of the Q-ADDS (Queensland Adult Deterioration Detection System) training, which should be comprehensive and mandatory, and include what to do when you recognize and respond to clinical deterioration. In this training, they will focus on the interpretation of Q-ADDS scores, and how the deterioration thresholds are breached when followed by required clinical escalation protocols. However, hospital can establish and ensure early intervention by thoroughly educating staff on both the application of the Q-ADDS tool and mandatory steps for escalating the care. |
The expected outcome is improved adherence to the NSQHS Standard 8: and Acute Deterioration recognised and responded to, which underlines the need for the timely recognition of clinical deterioration and escalation of care. Use of Q-ADDS will aid in the proper detection of early physiological changes and correct protocols to prevent further deteriorating and reduce adverse outcomes (Le Lagadec et al., 2021). This training will enable staff to read Q-ADDS scores better and initiate prompt response interventions when needed, for better quality patient care. |
|
| Nursing intervention to make change. | Expected outcome of the Intervention. | Evaluation: How can this outcome be analysed in future. |
| Intervention 2: Implementation of ISBAR Protocol Communicating more clearly and structured in the healthcare settings is essential and ISBAR (Introduction, Situation, Background, Assessment, and Recommendation) communication tool is also introduced for all clinical handovers and change of shifts, especially for patients displaying signs of deterioration or with a high risk. ISBAR provides a framework for healthcare professionals to quickly pass along critical patient information and prevents gaps in communication that can create patient safety crises during transitions of care. |
In high stress situations with deteriorating patients, using the ISBAR format will allow healthcare teams to communicate vital data about a patient’s condition thereby reducing the risk of miscommunication (Burgess et al., 2020). Communication breakdowns were a big factor in the lack of escalations found in the Roy Jacobs case, according to coroner's findings. With ISBAR, clinical handovers are standardized, and the information being passed on between nursing and medical teams becomes clearer and timelier decisions are made (Chien et al., 2022). This is expected to result in a significant improvement in communication quality during handovers and ultimately in patient safety, error reduction and speed of interventions to respond to patient deterioration. Moreover, ISBAR aligns with the NSQHS Standard 6: Effective communication at critical patient care points: communicating for safety. |
The ISBAR can then be evaluated through handover audits, staff feedback, and monitoring patient outcomes. Signs of success are a reduction in communication failures leading to incident and improved response times for deteriorating patients. See Australian health protocols, including those provided by the Australian Commission on Safety and Quality in Health Care for further information on implementing ISBAR. |
| Nursing intervention to make change. | Expected outcome of the Intervention. | Evaluation: How can this outcome be analysed in future. |
| Intervention 3: Real-Time Escalation Monitoring and Feedback System Clinical escalation protocols are demonstrated to be critical compliance monitors in the setting of patient deterioration and real time monitoring is a critical tool for such monitoring (Anstey et al., 2019). This system will capture key data, such as the frequency of rapid response team activations, usage of early warning tools like Q-ADDS, and adherence to NSQHS Standard 8: Acute Deterioration – Recognition and Response. Healthcare teams can look at these metrics continuously and if they find deviations from the procedures needed for escalation, they get instant feedback on how they can close any gaps in practice. |
The result is expected to be improved real time adherence to escalation protocols with staff promptly reacting when patient deterioration is detected. Monitoring system will provide continuous feedback to healthcare providers to change their practices where necessary to improve safety of patients and preventing adverse outcomes due to delayed escalations (Considine et al., 2021). Its further contribution will be in the culture of accountability and ongoing education by allowing staff to learn from past events and make their clinical decisions better. |
This intervention will be successful, measured by real time data analysis related to patient outcomes, escalation rates and rapid response activations. Throughout the study, the monitoring system will generate monthly reports which will then be reviewed by clinical leaders for continuous quality improvement. Effectiveness of the system will be proven by the decrease of the number of incidents connected with missed escalations or delayed responses. |
Anstey, M. H., Bhasale, A., Dunbar, N. J., & Buchan, H. (2019). Recognising and responding to deteriorating patients: what difference do national standards make?. BMC health services research, 19, 1-7. https://link.springer.com/article/10.1186/s12913-019-4339-z
Augutis, W., Flenady, T., Le Lagadec, D., & Jefford, E. (2023). How do nurses use early warning system vital signs observation charts in rural, remote and regional health care facilities: A scoping review. Australian Journal of Rural Health, 31(3), 385-394. https://onlinelibrary.wiley.com/doi/pdf/10.1111/ajr.12971
Australian Commission on Safety and Quality in Health Care (2024) Clinical governance standard, Clinical Governance Standard | Australian Commission on Safety and Quality in Health Care. https://www.safetyandquality.gov.au/standards/nsqhs-standards/clinical-governance/clinical-governance-standard.
Australian Commission on Safety and Quality in Health Care (2024b) Communicating for Safety Standard, Communicating for Safety Standard | Australian Commission on Safety and Quality in Health Care. https://www.safetyandquality.gov.au/standards/nsqhs-standards/communicating-safety-standard
Australian Commission on Safety and Quality in Health Care (2024c) Recognising and responding to acute deterioration standard, Recognising and Responding to Acute Deterioration Standard | Australian Commission on Safety and Quality in Health Care. https://www.safetyandquality.gov.au/standards/nsqhs-standards/recognising-and-responding-acute-deterioration-standard
Burgess, A., Van Diggele, C., Roberts, C., & Mellis, C. (2020). Teaching clinical handover with ISBAR. BMC medical education, 20, 1-8. https://link.springer.com/article/10.1186/s12909-020-02285-0
Chien, L. J., Slade, D., Dahm, M. R., Brady, B., Roberts, E., Goncharov, L., ... & Thornton, A. (2022). Improving patient‐centred care through a tailored intervention addressing nursing clinical handover communication in its organizational and cultural context. Journal of advanced nursing, 78(5), 1413-1430. https://doi.org/10.1111/jan.15110
Considine, J., Fry, M., Curtis, K., & Shaban, R. Z. (2021). Systems for recognition and response to deteriorating emergency department patients: a scoping review. Scandinavian journal of trauma, resuscitation and emergency medicine, 29(1), 69. https://link.springer.com/article/10.1186/s13049-021-00882-6
Le Lagadec, M. D., Dwyer, T., & Browne, M. (2021). Patient Deterioration in Australian Regional and Rural Hospitals: Is the Queensland Adult Deterioration Detection System the Criterion Standard?. Journal of Patient Safety, 17(8), e1879-e1883. https://www.researchgate.net/profile/Marie-Le-Lagadec/publication/343008409_VALIDATING_THE_QUEENSLAND_ADULT_DETERIORATION_DETECTION_SYSTEM_Q-ADDS/links/5f16c07392851cd5fa39b6c8/VALIDATING-THE-QUEENSLAND-ADULT-DETERIORATION-DETECTION-SYSTEM-Q-ADDS.pdf
Park, S.A. and Kellerman, T. (2024) Acute nursing care: Recognition and response to deteriorating patients, ANMJ. https://anmj.org.au/acute-nursing-care-recognition-and-response-to-deteriorating-patients/ .
Are you confident that you will achieve the grade? Our best Expert will help you improve your grade
Order Now